Preventing Pressure Sores: Essential Tips for Wheelchair Users
Pressure sores can be painful and can lead to serious complications, such as infection, sepsis, and even death. Therefore, it is important for wheelchair users to take steps to prevent pressure sores.
Wheelchair users are at an increased risk of developing pressure sores because they are often sitting for long periods of time. The pressure from sitting can cause the skin to break down, especially in areas where there is bony prominence, such as the hips, buttocks, and heels.
Section 1
Understanding Pressure Sores - Causes and Risk Factors
Pressure sores are a significant concern for wheelchair users as they can affect skin health and overall well-being. These sores develop due to sustained pressure on specific areas of the body, leading to reduced blood flow and tissue damage. Understanding the causes and risk factors associated with pressure sores is essential for wheelchair users and caregivers to implement preventive measures effectively. By understanding these causes and risk factors, wheelchair users and caregivers can take proactive measures to prevent pressure sores.
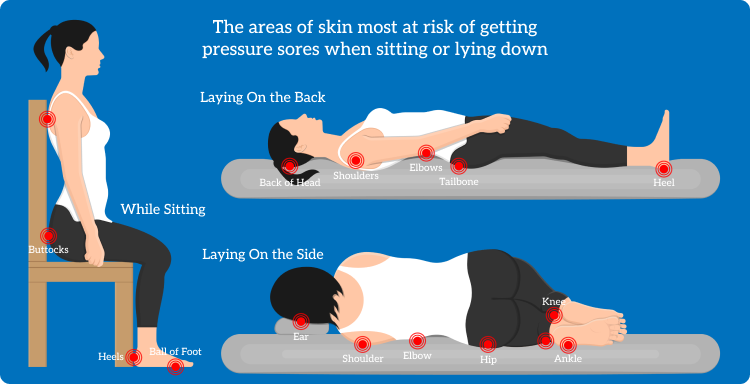
The areas of skin most at risk of pressure sores
Causes of Pressure Sores
Prolonged Pressure: Prolonged periods of sitting or lying in the same position exert continuous pressure on particular body areas, especially bony prominences like the hips, tailbone, heels, and shoulder blades. Over time, this pressure can compromise blood flow, leading to tissue breakdown and pressure sore formation.
Friction and Shear: Friction occurs when the skin rubs against a surface, like the wheelchair seat, while shear refers to the skin’s movement in one direction while the underlying bone moves in the opposite direction – for example, when a bed is elevated at the head, the weight of the body may cause the tailbone to move down in the bed while the skin over the bone may stay in place. These forces can cause skin damage and make the skin more susceptible to pressure sores.
Moisture and Incontinence: Excessive moisture, such as sweat or incontinence, can soften the skin, making it more vulnerable to damage. When the skin is moist, it is more likely to suffer from friction and abrasion, increasing the risk of pressure sores.
Poor Nutrition: Adequate nutrition is crucial for skin health and tissue repair. A diet lacking in essential nutrients, especially proteins, vitamins, and minerals, can impair the body’s ability to withstand pressure and heal effectively.
Risk Factors for Pressure Sores
Immobility: Wheelchair users, who often have limited mobility, are at a higher risk of pressure sores due to the inability to change positions independently. This immobility leads to sustained pressure on certain body areas, increasing the likelihood of pressure sore development.
Sensory Impairment: Individuals with sensory issues, such as those with spinal cord injuries or neurological conditions, may have difficulty sensing discomfort or pain in pressure-prone areas. As a result, they might not be aware of the need to adjust their positions to relieve pressure, leading to an increased risk of pressure sores.
Age: Advanced age can be a contributing factor to pressure sore development. Older adults may have thinner skin and reduced blood circulation, making their skin more susceptible to damage and slower to heal.
Chronic Health Conditions: Certain medical conditions, like diabetes and vascular disease, can compromise blood flow and impede the healing process, increasing the risk of pressure sores.
Poor Circulation: Individuals with circulatory problems face a higher risk of pressure sores due to reduced blood flow. Impaired circulation hinders the body’s ability to deliver nutrients and remove waste products from tissues, leading to tissue breakdown and pressure sore development.
Section 2
Recognising the Stages of Pressure Sores
Pressure sores, in their initial stages, may appear as seemingly harmless red patches on the skin. However, it’s crucial to recognise and understand the different stages of pressure sores to take timely action and prevent further progression. Pressure sores are generally categorised into 6 categories, each with distinct characteristics, symptoms, and potential complications:
Stage 1 pressure sores (also known as ‘Non-Blanchable Pressure Sores’) are characterised by localised areas of skin discoloration, often appearing as red, pink or purple patches on the skin.
The affected skin area may feel warmer or cooler to touch than the surrounding areas. At this stage the skin is still intact and there is no visible open wound.
If identified at this stage, prompt intervention can prevent the sore from advancing and developing into a more severe stage.
Stage 2 pressure sores (also known as ‘Partial Thickness Skin Loss Pressure Sores’) involve, as the name suggests, partial-skin loss. The affected area may appear as an open wound or blister.
The wound will be tender and painful, with redness and swelling potentially present around the damaged skin area.
Without proper care, stage 2 pressure sores can progress and cause further tissue damage.
Stage 3 pressure sores (also known as ‘Full Thickness Skin Loss Pressure Sores’) involve full thickness skin loss. The damaged area extends beyond the outer layer of skin into the underlying tissue, creating a deeper ulcer.
The ulcer may look like a small crater with visible fat tissue, there may also be a foul odour present.
Stage 3 pressure sores are at a high risk of infection and require immediate medical attention to prevent very serious complications.
Stage 4 pressure sores (also known as ‘Full Thickness Tissue Loss Pressure Sores’) are the most severe and involves extensive tissue damage and will have exposed bone, tendons or muscle.
The wound is likely to expose muscle, tendons and even bones an there may be significant amounts of dead tissue present.
Stage 4 pressure sores can lead to severse infections, affection both the skin and deeper tissues. They can also be life threatening and require intensive medical treatment.
In some instances, pressure sores are designated as ‘unstageable’ if the full extent of tissue damage cannot be observed due to the presence of slough (yellow, tan, grey or brown dead tissue) or eschar (hardened blackened tissue) covering the wound.
In these instances, medical professionals need to remove the dead tissue in order to assess and treat the wound appropriately.
Recognising the stages of pressure sores is crucial for prompt intervention and preventing any further deterioration.
Section 3
Importance of Proper Seating and Positioning
For wheelchair users especially, proper seating positioning is a critical aspect of pressure sore prevention and overall comfort. By understanding the significance of correct seating and positioning, individuals can alleviate pressure on vulnerable areas, reduce the risk of pressure sores, and enhance their overall well-being.
In this section, we will delve into why proper seating positioning matters and explore strategies to achieve optimal posture, weight distribution, and regular position changes.
Alleviating Pressure on Vulnerable Areas
Proper seating positioning aims to distribute pressure evenly across the body, reducing the concentrated force on specific bony prominences. Wheelchair users typically spend prolonged periods in their chairs, making it crucial to avoid excessive pressure on regions like the hips, tailbone, heels, and shoulder blades.
Optimal Posture
Achieving and maintaining optimal wheelchair posture is fundamental for the well-being and overall health of wheelchair users. Proper posture not only helps prevent pressure sores but also ensures better support for the spine, reduces the risk of musculoskeletal issues, enhances respiratory function, and promotes overall comfort.
Spinal Alignment
Maintaining proper spinal alignment is crucial for wheelchair users. The spine should be in a natural and neutral position, with the head aligned over the shoulders, and the shoulders aligned over the hips. Avoiding slouching or excessive leaning to one side can prevent unnecessary pressure on the spinal column and reduce the risk of back pain and discomfort.
Pelvic Positioning
Proper positioning of the pelvis is essential for supporting the spine and maintaining stability. Wheelchair users should aim to keep their pelvis in a neutral position, with the pelvis level and the weight evenly distributed on both sides. This helps prevent the development of pressure sores on the hips and tailbone and provides a solid foundation for optimal posture.
Lower Extremity Alignment
The alignment of the lower extremities plays a vital role in wheelchair posture. The knees should be at approximately 90 degrees, with the feet resting flat on the footrests. Proper foot positioning helps distribute weight evenly and prevents excessive pressure on the heels or other areas of the feet.
Upper Extremity Alignment
Positioning of the upper extremities is important for maintaining balance and facilitating functional tasks. The arms should be relaxed, with the elbows positioned at approximately 90 degrees and resting comfortably on the armrests. Avoiding excessive leaning on the armrests can help reduce pressure on the elbows and forearms.
Head & Neck Support
Proper head and neck support are essential for comfort and maintaining an open airway. Wheelchair users should ensure that their head is supported and aligned with the spine. Pillows or appropriate headrests can be used to provide additional support and reduce the risk of neck strain.
Distributing Weight Effectively
Even weight distribution is a key principle in achieving optimal wheelchair posture. Regularly shifting weight and performing weight shifts from side to side help prevent pressure on specific body areas. Utilizing pressure relief techniques and making slight adjustments to seating positions throughout the day can significantly reduce localized pressure and promote blood flow.
Regular Position Changes
Encouraging regular position changes is vital for preventing stiffness and discomfort. Wheelchair users should aim to change their positions every hour or more frequently, depending on individual needs. Performing small adjustments to the seating position and incorporating brief stretching exercises can enhance overall comfort and reduce the risk of pressure sores.
By maintaining optimal wheelchair posture, individuals can enjoy improved comfort, reduced risk of pressure sores, and better overall health. Consistently adhering to proper spinal alignment, pelvic positioning, lower and upper extremity alignment, and head and neck support can go a long way in enhancing the well-being and quality of life of wheelchair users. In the following section, we will focus on the process of selecting the right wheelchair cushion, considering essential factors that aid in pressure relief and prevention.
Section 4
Choosing the Right Wheelchair Cushion
Selecting the right wheelchair cushion is a crucial step in enhancing comfort, promoting proper posture, and preventing pressure sores for wheelchair users. With a wide range of cushions available, understanding the key factors that contribute to pressure relief and prevention is essential.
Material & Constuction
The material and construction of the wheelchair cushion significantly impact its performance. Common materials include foam, gel, air, and combination cushions. Foam cushions provide stable support and comfort, while gel cushions offer excellent pressure redistribution properties. Air cushions can be adjusted to individual preferences and provide dynamic support, reducing the risk of pressure sores.
Pressure Redistribution
The primary goal of a wheelchair cushion is pressure redistribution. Look for cushions specifically designed to distribute pressure evenly across the seating surface. This helps alleviate pressure on vulnerable areas and reduces the risk of developing pressure sores.
Cushion Size and Shape
Choosing the right size and shape of the cushion is essential for achieving optimal support and positioning. Wheelchair users should consider their body size and wheelchair dimensions to ensure the cushion fits properly and provides adequate support to the entire seating area.
Weight Capacity
Check the weight capacity of the cushion to ensure it can support the user’s weight comfortably. It’s important to select a cushion that can support the individual’s weight without compromising its pressure relief capabilities.
Cushion Cover
The cushion cover plays a significant role in maintaining hygiene and preventing moisture buildup. Choose a cover that is breathable, easy to clean, and provides protection against spills and moisture.
Mobility and Lifestyle Considerations
Consider the user’s mobility and lifestyle when choosing a wheelchair cushion. For individuals who require frequent transfers, a lightweight and portable cushion may be preferable. Additionally, consider the ease of maintenance and whether the cushion can withstand everyday use and transportation.
Selecting the right wheelchair cushion is a crucial step in enhancing comfort, promoting proper posture, and preventing pressure sores for wheelchair users. With a wide range of cushions available, understanding the key factors that contribute to pressure relief and prevention is essential.
Section 5
Skin Care and Hygiene Practices
Proper skin care and hygiene practices are vital for wheelchair users to maintain healthy skin, prevent pressure sores, and reduce the risk of skin infections. As wheelchair users may have limited mobility, paying close attention to skin health is crucial in preserving comfort and overall well-being.

Cleansing the Skin
Regular cleansing of the skin is essential for removing sweat, dirt, and bacteria that can accumulate throughout the day. Use mild, pH-balanced soaps or cleansers when bathing or washing. Gently pat the skin dry with a soft towel after washing, avoiding harsh rubbing that could damage the skin’s delicate surface.
Moisturising the Skin
Keeping the skin well-hydrated is essential for preventing dryness and maintaining its integrity. Apply a fragrance-free and hypoallergenic moisturizer regularly to prevent skin dryness and cracking. Pay particular attention to pressure-prone areas and ensure the moisturizer is fully absorbed into the skin.
Inspecting the Skin
Performing regular skin inspections is crucial in identifying any early signs of pressure sore development. Wheelchair users should inspect their skin thoroughly, paying close attention to areas that are susceptible to pressure sores, such as the buttocks, hips, heels, and elbows.
Managing Incontinence
For individuals managing incontinence, maintaining good skin hygiene is vital. Promptly change soiled undergarments and clothing to avoid prolonged skin exposure to moisture, which can lead to skin breakdown. Use barrier creams or ointments to protect the skin from the irritating effects of urine or feces.
Avoid Harsh Products and Irritants
Minimise the use of harsh products or chemicals that can irritate the skin. Avoid scented products, as they may contain ingredients that can cause skin reactions. Opt for products labeled as “hypoallergenic” or “fragrance-free” to reduce the risk of skin irritation.
Practicing Pressure Relief Techniques
Incorporating regular pressure relief techniques into daily routines can significantly reduce the risk of pressure sores. Encourage wheelchair users to perform weight shifts, lean side to side, and change positions regularly to alleviate pressure on vulnerable areas.
Maintain Proper Nutrition
A balanced and nutritious diet is essential for skin health. Adequate intake of vitamins, minerals, and protein supports the body’s ability to repair and maintain healthy skin. Encourage a diet rich in fruits, vegetables, lean proteins, and whole grains.
Seeking Professional Guidance
For individuals with specific skin conditions or concerns, seeking guidance from healthcare professionals, such as dermatologists or wound care specialists, is beneficial. They can provide tailored advice on managing skin issues and preventing pressure sores effectively.
Section 6
Daily Pressure Relief Techniques
Daily pressure relief techniques are integral to preventing pressure sores and maintaining optimal skin health for wheelchair users. These techniques aim to alleviate pressure on vulnerable areas, promote blood circulation, and reduce the risk of skin breakdown. In this section, we will present a range of effective pressure relief techniques and exercises that can be easily incorporated into daily routines.
Weight Shifts
Regular weight shifts are effective in reducing pressure on specific body areas. Encourage wheelchair users to shift their weight from one side to the other every 15-20 minutes. They can achieve this by leaning slightly to the left or right, effectively distributing pressure and providing relief to pressure-prone regions.
Leaning Forward and Backward
Leaning forward and backward in the wheelchair helps to redistribute pressure on the buttocks, thighs, and other sensitive areas. Wheelchair users can lean forward slightly, using their arms to support the upper body, and then lean backward to alternate and relieve the pressure distribution.
Tilting the Wheelchair
Many wheelchairs come with the option to tilt, allowing users to change their seating position and reduce pressure on the buttocks and lower back. Tilting the wheelchair backward redistributes pressure to the backrest while tilting it forward relieves pressure from the buttocks.
Utilising Pressure Relief Cushions
Pressure relief cushions are specially designed to distribute pressure more evenly across the seating surface. These cushions often incorporate materials like foam, gel, or air to provide optimal support and pressure relief. Wheelchair users can benefit from using pressure relief cushions to prevent pressure sores and enhance overall comfort.
Frequent Repositioning
Changing positions frequently throughout the day is key to preventing pressure sores. Encourage wheelchair users to reposition themselves in the chair by adjusting the backrest angle, elevating the footrests, or shifting their weight to different areas of the seating surface.
Monitoring Sitting Time
Limiting the amount of time spent sitting is essential for maintaining skin health and reducing the chance of eveloping pressure sores. Encourage wheelchair users to take regular breaks from sitting by performing short standing or stretching exercises, if possible.
Section 7
Lifestyle Factors - Nutrition, Exercise, and Lifestyle Choices
Beyond specific wheelchair-related practices, incorporating healthy lifestyle factors can play a significant role in preventing pressure sores and promoting overall well-being for wheelchair users. Proper nutrition, regular physical activity, and making conscious lifestyle choices are essential components in maintaining healthy skin and reducing the risk of pressure sore development.
A balanced and nutritious diet is vital for maintaining healthy skin and supporting the body’s ability to heal and prevent pressure sores. Incorporating a variety of fruits, vegetables, whole grains, lean proteins, and healthy fats provides essential nutrients for skin health and overall immune function. Adequate protein intake is particularly important for tissue repair and regeneration.
Staying well-hydrated is crucial for skin moisture and elasticity. Drinking an adequate amount of water throughout the day helps prevent skin dryness, which can make the skin more susceptible to damage and pressure sore development. Encourage wheelchair users to have water within reach and maintain proper hydration.
Even with limited mobility, regular physical activity is essential for promoting circulation, muscle strength, and overall health. Encourage wheelchair users to engage in appropriate exercises and activities tailored to their abilities. These can include wheelchair sports, stretching exercises, and activities that promote upper body strength.
Maintaining a healthy weight is beneficial for reducing pressure on vulnerable areas and minimizing the risk of pressure sores. For individuals who have limited mobility, managing weight becomes even more crucial in preventing excessive pressure on specific body regions.
Certain lifestyle choices can increase the risk of pressure sore development. Wheelchair users should avoid harmful habits such as smoking and excessive alcohol consumption, as these can impair blood circulation and hinder the body’s natural healing processes.
In addition to proper nutrition and exercise, protecting the skin from external factors is essential. Wheelchair users should use sunscreen when outdoors to prevent sunburn, which can damage the skin and increase the risk of pressure sores. Wearing appropriate clothing that provides skin protection is also beneficial.
Encourage wheelchair users to elevate their legs periodically to promote blood circulation. Raising the legs can help reduce swelling, support circulation, and prevent pressure sores on the heels and lower legs.
By adopting these lifestyle factors and incorporating them into their daily lives, wheelchair users can significantly reduce the risk of pressure sores and enhance their overall quality of life. Proper nutrition, regular physical activity, and positive lifestyle choices are essential components in maintaining healthy skin, promoting comfort, and reducing the likelihood of pressure sore development. In the concluding section of this article, we will summarize the key points discussed and emphasize the significance of implementing preventive measures to avoid pressure sores for wheelchair users.
Conclusion
Incorporating preventive measures is vital for wheelchair users to avoid pressure sores and maintain skin health. Understanding risk factors, utilizing proper seating and cushioning, and adopting daily pressure relief techniques are key steps. Additionally, practicing good skin care, embracing a balanced diet, and engaging in regular physical activity play crucial roles in preventing pressure sores. By prioritizing these essential tips, wheelchair users can lead comfortable and healthy lives, free from the challenges of pressure sores.



 Customer reviews
Customer reviews
